Investigating the Effect of Temperature on the Efficacy of Agicoat© Silver Nanocrystal Dressing Through Its Impact on Staphylococcus aureus Under Varying Temperature Conditions
Keywords:
Agicoat© silver nanocrystal dressing, Staphylococcus aureus, ambient temperatureAbstract
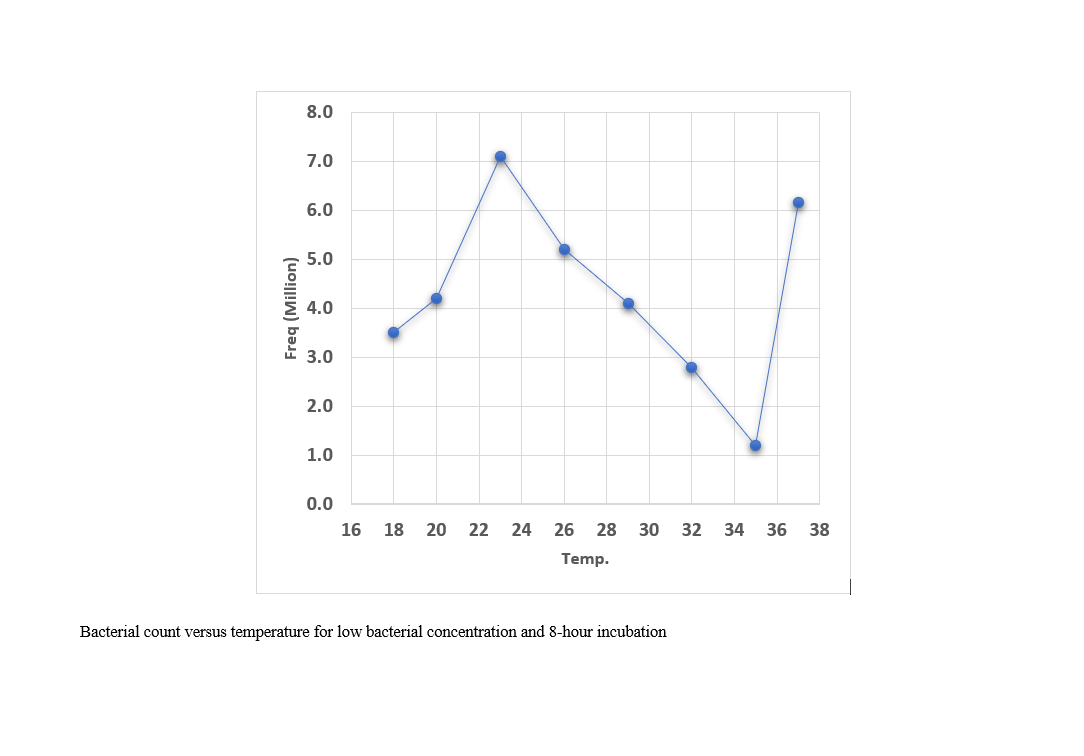
In a case study, the results of two experiments conducted at 30 °C and 37 °C demonstrated that Agicoat© silver nanocrystal dressing exhibits enhanced performance in eliminating microbial agents at 37 °C. This observation gave rise to the hypothesis that regulating the environmental temperature may serve as a method to reduce the duration of treatment—an aspect that has been largely overlooked in current therapeutic approaches. According to the recommendations of the U.S. Centers for Disease Control and Prevention (CDC), the standard temperature advised for patient hospital rooms is 24 °C, and in general, physicians do not incorporate room temperature as a variable in treatment protocols. Therefore, in this study, through laboratory experiments, we investigated the effect of increased ambient temperature on Agicoat© silver nanocrystal dressings, a product developed in Iran. After preparing dressing samples containing microbes at three concentrations—low, high, and no microbial presence—they were incubated for durations of 8 and 24 hours at various temperatures ranging from 18 °C to 37 °C. The investigation was conducted in two parts: a chemical assessment measuring silver ion release, and a microbiological assessment measuring the bactericidal efficacy against Staphylococcus aureus. The findings of this study led to the formulation of a protocol for adjusting the room temperature in patient care settings. By doing so, the treatment duration can be reduced, which in turn shortens hospitalization time, increases healthcare efficiency, reduces the financial burden on health insurance systems, and helps address the national shortage of hospital beds.
References
H. Jangid, S. Singh, P. Kashyap, A. Singh, and G. Kumar, "Advancing biomedical applications: An in-depth analysis of silver nanoparticles in antimicrobial, anticancer, and wound healing roles," Frontiers in Pharmacology, vol. 15, p. 1438227, 2024.
M. Harun-Ur-Rashid, T. Foyez, S. B. N. Krishna, S. Poda, and A. B. Imran, "Recent advances of silver nanoparticle-based polymer nanocomposites for biomedical applications," RSC advances, vol. 15, no. 11, pp. 8480-8505, 2025.
N. Barua and A. K. Buragohain, "Therapeutic Potential of Silver Nanoparticles (AgNPs) as an Antimycobacterial Agent: A Comprehensive Review," Antibiotics, vol. 13, no. 11, p. 1106, 2024.
S. Hadi and O. Omar, "Antibacterial effect and biocompatibility of silver nanoparticle-coated bone allograft substitutes," Cellular and Molecular Biology, vol. 70, no. 3, pp. 67-77, 2024.
B. M. Abdallah, P. Rajendran, and E. M. Ali, "Potential treatment of dermatophyte trichophyton rubrum in rat model using topical green biosynthesized silver nanoparticles with achillea santolina extract," Molecules, vol. 28, no. 4, p. 1536, 2023.
W. McGuiness, E. Vella, and D. Harrison, "Influence of Dressing Changes on Wound Temperature," Journal of Wound Care, 2004, doi: 10.12968/jowc.2004.13.9.26702.
W. McGuiness and E. V. D. Harrison, "Influence of dressing changes on wound temperature," Journal of Wound Care, vol. 13, no. 9, 2013, doi: 10.12968/jowc.2004.13.9.26702.
L. Y. Zhu et al., "Advances in the research of the relationship between wound temperature and wound healing," Chinese journal of burns (Zhonghua Shao Shang Za Zhi), vol. 34, no. 11, p. 5, 2018.
M. D. Sheldon V. Pollack, "Environmental Factors Affecting Wound Healing," J. Dermatol. Surg. Oncol., vol. 5, no. 6, 1973, doi: 10.1111/j.1524-4725.1979.tb00699.x.
P. Cuthbertson D and J. Tilstone W, "Effect of Environmental Temperature on The Closure of Full Thickness Skin Wounds in The Rat," the Department of Pathological Biochemistry, University and Royal Infirmary, Glasgow, Quart. J. exp. Physiol., vol. 52, pp. 249-257, 1967, doi: 10.1113/expphysiol.1967.sp001910.
M. D. Alfred Large and M. D. Peter Heinbecker, "The Effect of Cooling on Wound Healing," Annuals of Surgery, vol. 120, no. 5, 1944, doi: 10.1097/00000658-194411000-00005ER -.
M. E. Astaneh and N. Fereydouni, "Silver Nanoparticles in 3D Printing: A New Frontier in Wound Healing," ACS Omega, vol. 9, no. 40, pp. 41107-41129, 2024/10/08 2024, doi: 10.1021/acsomega.4c04961.
R. Qu, M. Chen, J. Liu, Q. Xie, N. Liu, and F. Ge, "Blockage of ATPase-mediated energy supply inducing metabolic disturbances in algal cells under silver nanoparticles stress," Journal of Environmental Sciences, vol. 131, pp. 141-150, 2023.
B. Sahoo et al., "Photocatalytic activity of biosynthesized silver nanoparticle fosters oxidative stress at nanoparticle interface resulting in antimicrobial and cytotoxic activities," Environmental Toxicology, vol. 38, no. 7, pp. 1577-1588, 2023.
M. Noga, J. Milan, A. Frydrych, and K. Jurowski, "Toxicological aspects, safety assessment, and green toxicology of silver nanoparticles (AgNPs)—critical review: state of the art," International Journal of Molecular Sciences, vol. 24, no. 6, p. 5133, 2023.
F. M. Aldakheel, M. M. E. Sayed, D. Mohsen, M. H. Fagir, and D. K. El Dein, "Green synthesis of silver nanoparticles loaded hydrogel for wound healing; systematic review," Gels, vol. 9, no. 7, p. 530, 2023.
S. K. Mallineni et al., "Silver nanoparticles in dental applications: A descriptive review," Bioengineering, vol. 10, no. 3, p. 327, 2023.
J. Wang, W. Jiang, J. Liang, and S. Ran, "Influence of silver nanoparticles on the resin-dentin bond strength and antibacterial activity of a self-etch adhesive system," The Journal of Prosthetic Dentistry, vol. 128, no. 6, pp. 1363. e1-1363. e10, 2022.
S. Zainab, S. Hamid, S. Sahar, and N. Ali, "Fluconazole and biogenic silver nanoparticles-based nano-fungicidal system for highly efficient elimination of multi-drug resistant Candida biofilms," Materials Chemistry and Physics, vol. 276, p. 125451, 2022.
P. Punpeng, "The effect of nano-silver fluoride in remineralization on artificial dentine caries: an in vitro study," 2022.
T. Guo, D. Wang, and S. S. Gao, "Incorporating nanosilver with glass ionomer cement–a literature review," Journal of Dentistry, p. 105288, 2024.
A. U. M. P. Federica Paladini, "Antimicrobial Silver Nanoparticles for Wound Healing Application: Progress and Future Trends," Department of Engineering for Innovation, University of SalentoCY - Via Monteroni, 73100 Lecce, Italy, 2019, doi: 10.3390/ma12162540.
Downloads
Published
Submitted
Revised
Accepted
Issue
Section
License
Copyright (c) 2025 Majid Fathabadi (Author); Soroush Maddah (Corresponding author); Hamideh Barghamadi (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.